Theresa Brown’s new memoir
Healing: When a Nurse Becomes a Patient
In Stores Now
Amazon Barnes & Noble Books-A-Million Bookshop IndieBound Pittsburgh’s City of Asylum Bookstore
When an oncology nurse is diagnosed with cancer, she has to confront the most critical, terrified, and angry patient she’s ever encountered: herself.
New York Times bestselling author Theresa Brown tells a poignant, powerful, and intensely personal story about breast cancer in Healing. She brings us along with her from the mammogram that would change her life through her diagnosis, treatment, and recovery. Despite her training and years of experience as an oncology and hospice nurse, she finds herself continually surprised by the lack of compassion in the medical maze—just as so many of us have. Why is she expected to wait over a long weekend to hear the results of her cancer tests if they are ready? Why is she so often left in the dark about procedures and treatments? Where is the empathy from caregivers? At times she’s mad at herself for not speaking up and asking for what she needs but knows that anyone labeled a “difficult” patient risks getting worse care.
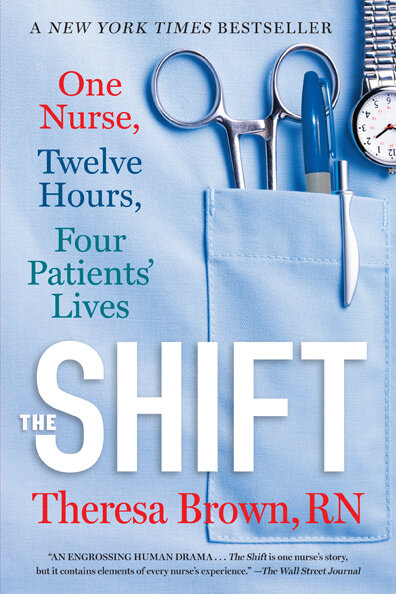
As she did in her book The Shift, Brown draws us into her work with the unforgettable details of her daily life—the needles, the chemo drugs, the rubber gloves, the frustrated patients—but from her new perch as a patient, she also takes a look back with rare candor at some of her own cases as a nurse and considers what she didn’t know then and what she could have done better. A must-read for all of us who have tried to find healing through our health-care system.
“Healing is a stunning book that helped me understand how to survive a serious illness and how to understand hospitals in general. Theresa Brown, RN, is also a hell of a good writer.” — James Patterson
“Deeply moving.” — Damon Tweedy, New York Times bestselling author of Black Man in a White Coat
“A smart, moving, clear-eyed, yet ultimately hopeful jewel of a read on health and care from one of the most thoughtful healthcare writers I know.” — Pauline W. Chen, MD, bestselling author of Final Exam: A Surgeon’s Reflections on Mortality

Theresa Brown
Nurse, Writer, and NY Times Bestselling Author of The Shift
Recent Columns & News
What Nurses Do: We Create Care
Cancer Nursing Today
June 2025
In this column I grapple with an issue that might seem beside the point of clinical work but actually matters a lot: the question of how to best define nursing. I’m writing about this because the International Council of Nurses (ICN) recently issued a new definition of what a nurse is, and although the definition is thorough and not incorrect, it ultimately fails to communicate the essence of nurses’ work, in part because it’s wordy and overly long.
Nursing and the Power of a Helping Hand
Cancer Nursing Today
May 2025
I’ve been lucky enough to live in Spain for the past three months1, and while I talk about nursing in this column, I need to set the stage in Spain first, so bear with me. This past weekend, my husband and I went for a hike at the Montserrat Monastery near Barcelona. You can see from the picture at left how stunning the monastery is, and my husband and I both marveled at why and how anyone would decide to build anything, much less the home for a religious community, in such a remote place.
Do Republicans want more mothers to die?
The Contrarian
May 2025
The United States has an abysmal maternal mortality rate: at 22.3 deaths per 100,000 live births, it is almost double the number of maternal deaths in the next country in line, Chile. For some perspective, consider that Norway’s rate in 2022 was 0. If you’re a Black woman in the United States, the likelihood of dying from a pregnancy-related cause is more than twice the U.S. rate overall: 49.5 deaths for every 100,000 births. And the maternal mortality rate here is getting worse, not better, which is why it’s beyond troubling that Republican legislators have called for huge cuts to Medicaid in their recent budget proposal.
About Theresa
Theresa Brown, PhD, BSN, RN, is a nurse and writer who lives in Pittsburgh. Her third book —Healing: When a Nurse Becomes a Patient — was published April 2022 and is available wherever books are sold. It explores her diagnosis of and treatment for breast cancer in the context of her own nursing work. Her book, The Shift: One Nurse, Twelve Hours, Four Patients' Lives, was a New York Times Bestseller.
Theresa has been a frequent contributor to the New York Times and her writing has appeared on CNN.com, and in The American Journal of Nursing, The Journal of the American Medical Association, and the Pittsburgh Post-Gazette. Theresa has been a guest on MSNBC Live and NPR’s Fresh Air. Critical Care: A New Nurse Faces Death, Life, and Everything in Between is her first book. It chronicles her initial year of nursing and has been adopted as a textbook in Schools of Nursing across the country.
Theresa's BSN is from the University of Pittsburgh, and during what she calls her past life she received a PhD in English from the University of Chicago. She lectures nationally and internationally on issues related to nursing, health care, and end of life. Becoming a mom led Theresa to leave academia and pursue nursing. It is a career change she has never regretted.
Available Now
Healing: When a Nurse Becomes a Patient
As an oncology and hospice nurse, I thought I knew cancer—knew it. But when I was diagnosed with cancer myself, I realized I knew nothing at all about being a cancer patient: how terrifying having cancer is, and how lonely. Healing: When a Nurse Becomes a Patient traces the intersection of my nurse-self and my patient-self, from breast cancer diagnosis through treatment and after, when I return to work in home hospice. What did Theresa-the-nurse learn from Theresa-the-patient? That we want and need compassion from our health care. Medicine can cure, but healing requires more: thoughtfulness, listening, and a genuine and generous focus on every patient.